Technology and Innovation – what I use now
Over the years, technology, advances in materials, and an understanding of the hip and knee joint has improved the overall revision rates in surgery. Often, patients have a concept that hip and knee replacements only last 10-15 years. In this article, we will go through some of the data, supported by the Australian National Joint Registry – a research tool that has collected almost all of the data from hip and knee replacements over the last 20 years.
HIP REPLACEMENTS

What is amazing is that there are 3231 different stem and acetabular combinations!
Hip replacements have been known to have one of the highest satisfaction rates of any surgical procedure performed in any specialty – making them an amazing way to restore function and remove pain. The method utilised with all of our hip replacements is using the Direct Anterior Approach and Patient Specific Technology.
The joint registry captures just under 700,000 hip replacements, with over 50,000 hip replacements being performed in 2019 alone.
The revision rate at 19 years is 10.6% meaning that approximately 1 in 10 patients would have undergone another procedure for their hip by 19 years after their procedure.


What factors affect the longevity of a total hip replacement?
Whilst none of this is an exact science, and there are many factors which go into determining why something survives forever, and some hip replacements don’t, there are some factors which were identified statistically as having an influence on longevity of a hip replacement.
Body mass indeX
When comparing BMI, patients who have a BMI over 30 have an elevated risk of revision. This increases further with the more elevated BMI’s with this who have a BMI over 40having twice the rate of revision than those with normal BMI (18.5-25). This data has only been collected however, for the last 4 years.
Medical comobidities
Patients are classified based on their medical risks/comorbidities and this is a factor in revision rates. Those who have chronic medical conditions have a higher risk of revision than healthy individuals.
AGE
The factor of age is not as large a factor as originally thought. Those under 55yo have a 12.9% chance of revision at 19 years, whilst those over 75 have a 9% chance.
As the years progress and our technologies improve, it appears that the overall revision rates are improving with more modern approaches to surgery, both with technology and understanding.
KNEE REPLACEMENTS

Interesting facts
There are 568 combinations of knee replacements used over the last 19 years.
The rate of cementing both components continues to increase

Traditionally knee replacement have not fared as well as total hip replacements in the literature. There is a slightly lower success rate when compared to hips. A knee is considered a more complex joint when compared to a hip joint.
Recently major changes in the number of surgeons adopting Kinematic alignment protocols has occurred that is not captured in the current data. The method of alignment of the knee replacement is something that is only recently becoming more relevant, as more studies are being produced to show the benefits of matching native alignment protocols.
There are more knee replacements than hip replacements performed with just under 850,000 knee replacements being assessed as part of the Joint Registry. Just under 67,000 knee replacements were performed in 2019
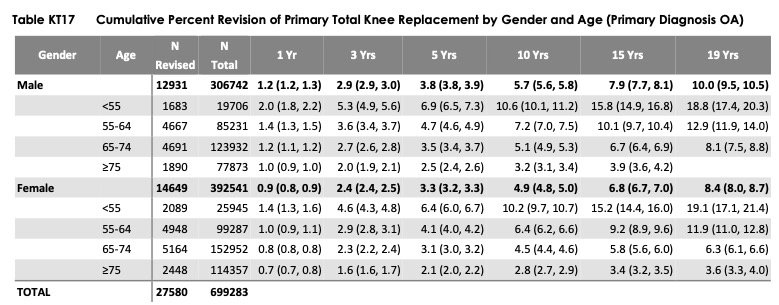
The longevity of knee replacements is also very good with a 9% revision rate at 19 years. The reason for revision in order of likelihood is: Loosening, Infection, Patellofemoral pain, Instability, Pain, Patella Erosion and Arthrofibrosis.
When age is considered, those under the age of 55yo have a 19% revision rate at 19 years, whilst those between 65-74 have a 7% revision rate. If you are over 75yo, you have a 3.8% revision rate.
Overall males have a slightly higher revision rate at 19 years, being 10% whilst females are 8.4%.
What factors affect the longevity of a total knee replacement?

Body mass index
Again, body mass index seems to feature as a factor in the longevity of an implant. As BMI increases, the chance of revision surgery increases. Again, this is data taken over the last 4 years only.
Medical comorbidities
As with the hip replacements above, patients with higher medical comobidities have a higher risk of revision surgery. This can be explained most likely by conditions such as diabetes, those on blood thinners etc.
Type of prosthesis design
According to the registry, the type of design of the implant has an impact on revision rates. The data is shown below.

WHAT TYPE OF SURGERY DOES DR CHIEN-WEN LIEW PERFORM

What methods will you receive with Dr Chien-Wen Liew
Dr Chien-Wen Liew has a dedicated practice in only total hip and total knee replacements. He no longer accepts new referrals for sports injury, trauma or other conditions of the hip and knee. This allows a dedicated focus to optimising all efforts towards a successful total hip replacemnt or total knee replacement.
total hip replacement
For over 8 years, all total hip replacements have been performed using the Direct Anterior Approach. This is an approach where no muscles or tendons are cut or detached during surgery. There are minimal restrictions, and early mobility. As part of the procedure, patient specific technology is utilised – meaning that a 3 dimensional scan is performed 2 months prior to surgery in order to create customised cutting jigs and accurate planning to ensure an accurate outcome and to decrease the amount of soft tissue damage during surgery. A specialised table is used during surgery to minimise touching any part of the leg except for the small operative field. During surgery an intra-operative scan is performed to double check that the procedure has matched with the Xrays, as well as the 3 dimensional plan as well as the individualised modelling. This ensures an accurate procedure in an effort to never return to the same hip again. There are no movement restrictions post operatively. Most procedures are performed under a spinal anaesthetic. No local anaesthetic is used during the procedure within the hip.
total knee replacement
The medial pivot design of the knee replacement has been a defining part of our practice. This allows the knee to glide in a natural movement. Combined with Kinematic Alignment, the procedure is now extremely planned using Patient Specific Technology. Kinematic alignment is where the final knee replacement is placed in a position to match a patient’s pre-arthritic anatomy rather than placed in what traditionally has been considered to be the “optimal” position for all patients. This means that each and every person will receive a position that mimics their own anatomy. Part of the benefit of this, is that there are no tendon, capsular, or ligamentous releases required, to balance the knee as we used to perform many years ago when each knee was aligned to be “straight”. This means that if you have been bow legged or knock kneed, pigeon toed or duck footed prior to developing knee osteoarthritis, then you will most likely be placed back into that position after surgery. This is done to regain the “forgotten knee” goal once recovery is completed. For every case, disposable instruments are used as part of the individualised patient equipment in order to decrease the risk of infection. We aim to walk our patients the same day, if surgery is performed in the morning, or first thing the following morning if performed in the afternoon. Most procedures are performed under a spinal anaesthetic. A nerve block is performed (adductor canal) in addition to a small amount of local anaesthetic at the back of the knee during surgery.
