Longevity of a Total Hip Replacement in 2023
Having covered this previously in 2016 this is an update with more indepth discussion about longevity as per the Australian Joint Replacement Registry. Whilst the registry is a tool to capture revisions, it does not capture patient satisfaction, or functional outcomes. So its use is to identify revision due to failures only. Due to this, its use should be more limited as a general discussion and should not take the place of discussions with myself or your doctor.
HIP REPLACEMENTS
GENERAL
The registry reports currently on 796,686 hip replacements performed up to the 31st of december 2021. That was an increase of 52,787 hip procedures than the same time the year before, Australia wide. Of that number, about 75% of them were total hip replacement, 10% were revisions, and 14% were partial hip replacements. Partial hip replacements are often performed in the context of hip fracture surgery rather than elective total hip replacements which I perform. Interestingly, revisions are declining as a percentage overall, with 12.9% being performed in 2003 compared to only 7.6% in 2021. This extrapolates to an improvement in techniques, and outcomes when revisions are concerned over many years, which is what is to be expected as we advance our understanding, accuracy and abilities. In this review today, we’ll also add some of the other criteria used to designate risk profiles, including ASA (Anaesthetic scoring for how healthy a patient is) and BMI (Body Mass Index).
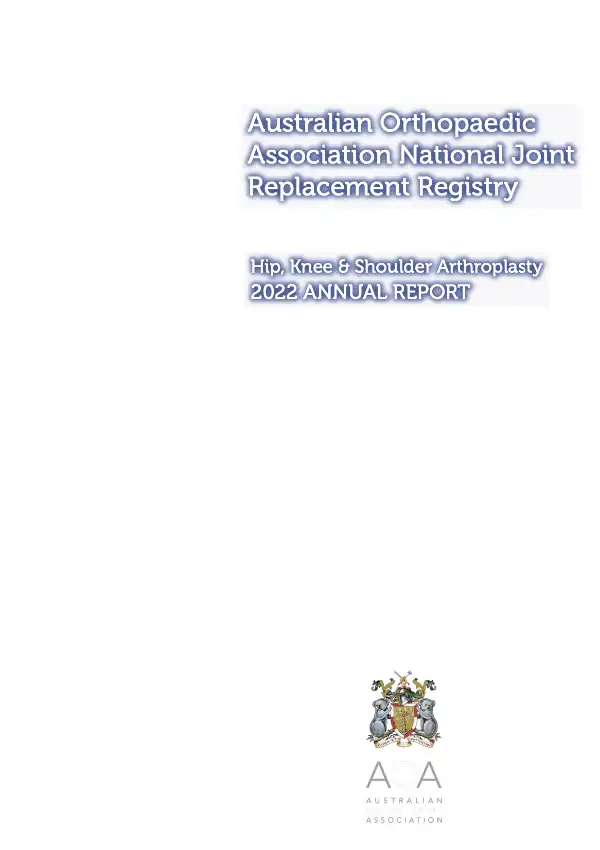
As can be seen from the above table, the revision rate in the context of total hip replacements for the purpose of osteoarthritis is excellent, with a 20 year revision rate of 8.4%. This means that at 20 years post procedure, 91.6% of all implants have not been revised which is an excellent result. When considering other causes for why a total hip replaement may be performed, the worst performer is most likely that for fractured neck of femurs (trauma) but that data is not out to 20 years as yet, as the trend for longevity in fracture patients is worse along the entire timeline up until the 15 year mark where it is marginally lower than that of osteonecrosis (death of the bone, usually the femoral head – also known as avascular necrosis). Those who have the surgery for Rheumatoid arthritis also have a higher revision rate over all, and interestingly, in the more complex sugery of developmental dysplasia of the hip, the revision rate is actually lower than that for osteoarthritis which is unusual and unexplained.
Why do implants get revised
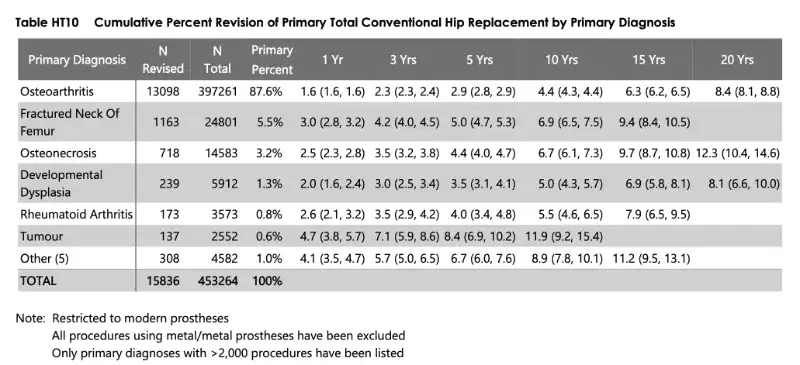
When considering the reasons for revision, we look to the reasons as designated by the surgeon. This means that for every revision, a surgeon has to allocate the revision to a particular category. In some cases, it is very simple (ie in the case of infection or dislocation/instability) but in some cases it can be hard – as in someone with unexplained pain that requires an exploration and revision. This means that these results can be somewhat inaccurate, but do act to help us understand the bulk of where revision are occuring and why. The most common reason for a revision was infection, consistuting 22% of cases, whilst prosthetic dislocation/instability accounted for 22%.
How does age affect revision rates
We know that being young is not preferred when performing a total hip replacement however, it is often unavoidable. Gone are the days when people are being told – wait until you are 60 or 65 until you have it done. These days, those “rules” are no longer effective, as they do not consider the patient as a whole – their quality of life, discomfort/pain, analgesic requirements and any impact that this may have on mental state, employment and general health deterioration. In the past, when longevity was not well knon or was actually considered to be poor, these rules may have saved someone’s mobility later, but in current times, prostheses and outcomes are fantastic as can be shown in the following table.

In the table above, you can see the number of patients revised as per age as a factor. So when we break down the 8.4% at 20 years, we can see that the best revision group is actually the >75yo group. On of the factors influencing this, is the life expectancy of the patient. Because those aged 55yo live longer, they will have a higher rate of revision. At 20 years, the revision rate for those under 55yo who have their total hip replacement for osteoarthritis is 9.3%. This is an excellent result, and shows how good joint replacements can be even at a younger age. Whilst we opt not to perform surgery too early, we do not use age as the predominant factor in deciding when to perform a total hip replacement on a patient will be.

Just for some interest, here I am showing the statistics based on gender. Interestingly here, the girls win here! They have an overall revision rate of 8% at 20 years compared to 9% at 20 years for men. The other interesting thing is that for men, the revision rate really doesn’t change. It is 9% overall, but is 9.3% for those under 55yo and 9% for those aged 65-75, whilst in females, it follows the trend more normally, where revision rates decrease as the patient is older, being 9% for those under 55yo and only 6.9% for those over 75yo.
The next prosthesis concept I wanted to discuss was dual mobility implants – these have been in place now for many years overseas, but came more as an option in Australia over the last 10 years – as a good way to increase stability in difficult cases and revisions for instability. Whilst they have a fantastic profile for instability, they have less of a known revision profile. Here we aim to look specifically at this, with the first 10 year data being available now, showing a slightly higher revision rate as compared to conventional components.
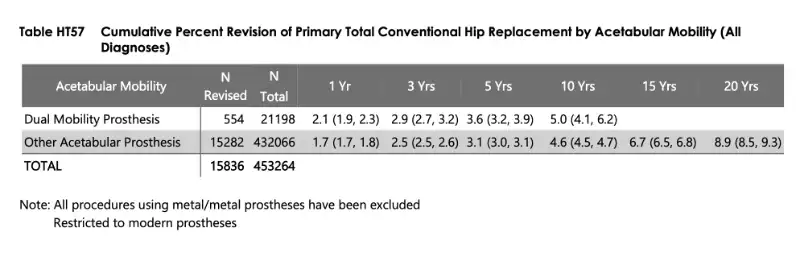
Here you can see a slightly higher revision rate at 10 years of 5% vs 4.6% for conventional prostheses. This is actually quite good, and should be considered exceptional given that most dual mobility implants are placed for those patients with higher than normal risks in general.
What patient factors effect the longevity of the hip replacement
The registry has only been collecting patient factors for a few years now, and not for the entire duration of the registry so data is not as robust as the standard demographic information above. But we do have some interesting findings here too. ASA is a score given to patients at the time of anaesthetic to designate the medical comorbidities and general risks of an anesthetic, with 1 given to the most healthy patients and 5 to the most unhealthy. In general, most patients undergoing hip replacements electively fall into the categories of ASA 1,2 or 3.
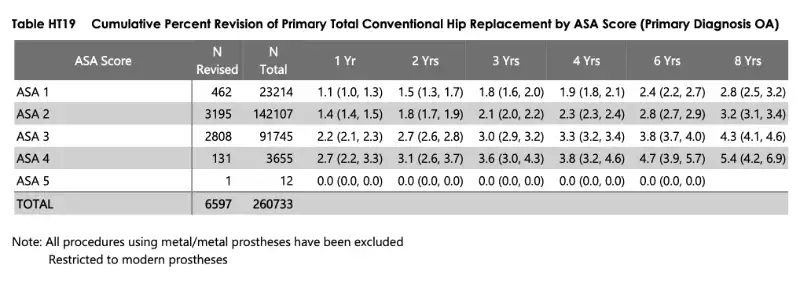
The above table is what we would expect from the data. At 8 years, the information suggests that those who have more medical comobidities and who are higher risk patients, go on to have a higher revision rate overall. This probably suggests that there are patient factors that either go into making the procedure more difficult, or the body’s response to the surgery more complex. Most likely this could be represented by conditions such as diabetes, and patients who smoke or are heavy alcohol drinkers, which will decrease the bodies ability to fight infection, and slow down wound healing, predisposition them to a higher risk of infection. When considering another interesting finding is the Body Mass Index (BMI) of a patient as well. This is a measure of height vs weight, and designates patients on a generalised score that isn’t perfect, but acts as a guide as to how healthy a patients weight may be for their height.

In this table above, we look at weight as a factor. For those patients who have elevated BMI, it appears as though there is a trend towards a higher revision. Elevated BMI patients are more difficult to perform technically due to the soft tissue envelope around the hip that may obscure the bony landmarks, and move soft tissue structures into less predictable areas – such as nerves and blood vessels. In addition to this, incising the apipose tissue creates a dead space which may act as an area where infection can accumulate. The results in the table above do show quite a significant increase in risk as the BMI extends over 35. In some hospitals, the limit for performing surgery on patients is a BMI under 40, which is now supported in the literature. When comparing the revision rate for those in a normal weight class to those in a BMI over 40 weight category, the revision rate is almost double the risk at 6 years. The data on this actually shows that elevated BMI patients have quite a higher risk of infection in those BMI 35 and over. In general, we would recommen patients to lose weight to get under the 35 BMI level before surgery if possible.
WHAT TYPE OF SURGERY DOES DR CHIEN-WEN LIEW PERFORM

What methods will you receive with Dr Chien-Wen Liew
Dr Chien-Wen Liew has a dedicated practice in only total hip and total knee replacements. He no longer accepts new referrals for sports injury, trauma or other conditions of the hip and knee. This allows a dedicated focus to optimising all efforts towards a successful total hip replacement or total knee replacement.
total hip replacement
For over 9 years, all total hip replacements have been performed using the Direct Anterior Approach. This is an approach where no muscles or tendons are cut or detached during surgery. There are minimal restrictions, and early mobility. As part of the procedure, patient specific technology is utilised – meaning that a 3 dimensional scan is performed 2 months prior to surgery in order to create customised cutting jigs and accurate planning to ensure an accurate outcome and to decrease the amount of soft tissue damage during surgery. A specialised table is used during surgery to minimise touching any part of the leg except for the small operative field. During surgery an intra-operative scan is performed to double check that the procedure has matched with the Xrays, as well as the 3 dimensional plan as well as the individualised modelling. This ensures an accurate procedure in an effort to never return to the same hip again. There are no movement restrictions post operatively. Most procedures are performed under a spinal anaesthetic. No local anaesthetic is used during the procedure within the hip.
Some general questions from our patients
Will there be cement used in my hip replacement?
In general no, I choose to use a cementless design for both the stem and the socket. This has a special coating called hydroxyapatite which is essentially like “artificial bone” where the pores are approximately 50 microns in size, enabling the native bone to grow into it. The prosthesis has a special macro structure which gives it immediate stbaility, so full weight bearing is possible as soon as you leave the operating theatre. For patients with significant osteoporosis, cement is generally used.
What will be bearing surface be made of?
For most hip replacements, we use a ceramic on ceramic articulation. This differs in some cases where a ceramic on polyethylene (plastic) is used. If your case has a specific risk of dislocation due to a connective tissue disorder such as ehlers danos syndrome or a neuromuscular disorder, then a dual mobility implant may be used, and this utilises a ceramic and plastic articulation.
Are there some circumstances where the direct anterior apporoach won't be used.
If you clinically have severe abductor deficiency (ie ruptured gluteal tendons completely), or you require specific posterior metalwork removal (such as a plate positioned for an acetabular fracture) or your anatomy requires an osteotomy to shorten the leg (such as in a severe case of dysplasia of the hip), then the direct anterior approach may not be the best for you. In these cases, I will refer you to one of my colleagues who can address these needs with a standard, posterior approach.
